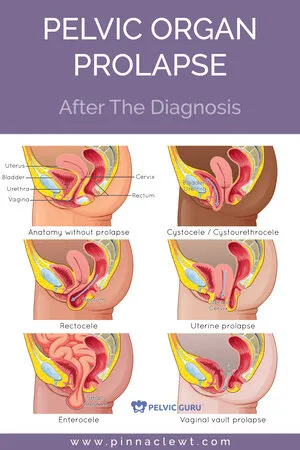
I’ve been asked by many women and patients over the years what they can do about their prolapse. They are often scared and also feel let down by their medical providers and society at large for NOT discussing the possibility of POP.
They are often told by their providers that things are not that bad and come back when it IS. Despite the fact that they are coming to their doctor to discuss their bothersome symptoms of feeling like things are falling out their pelvis or feeling pain and pressure with activities.
Overall, women are feeling VULNERABLE and HELPLESS.
Is this how the rest of life will be like??
The emotions in coming to terms with POP run DEEP. And the lack of knowledge about our options only makes it WORSE.
The two things that most women are aware of is…
-
Surgery
-
Kegels
Now these are not bad options, but they are often not necessary/needed or sufficient on their own, and are not the ONLY proactive options. Surgery may be needed, but if imbalances in the body remain unchanged that aggravate a prolapse, the surgery may not resolve symptoms long term. This is where the partnership between a surgeon and pelvic physical therapist specialist are a must.
Kegels. Contracting our pelvic floor muscles umpteen times a day is not an effective way to resolve a failure of pressure and can actually result in worse symptoms and pelvic pain.
So let’s talk about the OTHER OPTIONS. Most can be obtained with your pelvic physical therapist…
-
– Internal Support
-
– External Support
-
– Learning To Manage Intra-Abdominal Pressures Through Improving – – – Body Awareness, Coordination of the Deep Core Muscle TEAM.
-
– Pelvic and Hip STRENGTH.
-
– Manage Constipation and Other Toileting Tips
-
– Learning to MOVE and MINIMIZE PRESSURE
Internal Support
Internal supports are used intravaginally. If you have used a tampon, it’s not much different. So many women at first are really turned off by the idea until I put things into perspective…
If we had an unstable ankle and wanted to go for a hike, we would put on an ankle brace and wear a supportive shoe. THIS is the same thing for the pelvic floor.
A skilled doctor or nurse who has been trained can help fit a pessary. There are many shapes and sizes and the FIT IS EVERYTHING. When it fits properly, you should not be able to feel it or feel it shift with movement. I frequently refer patients for pessary fitting, and have specific providers I refer to in my area. If a provider tells a patient that they are only used to fitting older women for pessaries, I’d suggest you look for a new provider for this. Many younger women as early as in their 20’s successfully use pessaries.
External Support
If someone is really not able to use a pessary it is uncomfortable with the idea, an external support can be worn. It can be worn over undergarments and hides nicely under clothes. It provides a good amount of perineal compression/lift and is ideal for anyone who cannot wear a pessary, especially with more activity like running and exercise. One brace is called Braceability. Other garments that can be worn can be compression shorts such as volleyball shorts.
Learning to Manage Intra-abdominal Pressure Through Core Muscle Coordination and Strengthening
So many women are quite disconnected from their pelvic floor muscles. They do NOT have full command of this muscle group to be able to contract, relax and lengthen them. All three functions are needed to work properly. These muscles also need to be able to coordinate with the rest of the core muscle team including the diaphragm and deep abdominals.
A pelvic PT can help you get this back!
Pelvic and Hip Strength
The muscles of the pelvis and hips are all in the same neighborhood. Weakness of one group usually means the others are weak as well. However, sometimes, one muscle group will become over-tight to compensate for the other being too weak. A healthy balance of strength of the gluteals and pelvic floor is ESSENTIAL. Working with a pelvic PT should include this… NOT just kegels.
Constipation and Toilet Tips
Chronic constipation and having to strain to have a bowel movement can cause a prolapse over time. Even if this was not the cause, it will become ESSENTIAL to manage constipation from here on out. Supplements like Magnesium Citrate can help constipation as well as staying hydrated, healthy movement and exercise and a vegetable rich diet.
Three toilet tips include:
-
Using a stool at the toilet or Squatty Potty and splinting the perineum when having a bowel movement.
-
Splinting can be wadding a bit of toilet paper and using it to press upward over the perineum to provide some counter pressure and reduce the downward strain to the tissues. Many women find that this actually helps them void their bowel better.
-
DO NOT hold your breath while voiding your bowels. Breathing in and out slowly is the best way to NOT add too much strain to the pelvic floor.
Learning To Move and Minimize Pressure
There are a LOT of movements and activities that have the potential to majorly increase downward pressure on our pelvic floor. Getting up from a chair is a great example. TRULY managing POP HAS to include learning to move in a safer way and the term ‘pelvic safe” will be a part of your awareness.
Though it is seriously important to work with a skilled pelvic physical therapist individually, here are a couple of tips.
-
Exhale with Effort: if you are getting out of a chair, picking up a heavy item or child, breath OUT while you are on the move will encourage your core muscles to engage and provide more support for your pelvic floor.
-
While doing exercises (especially abdominal), monitor you belly for signs of too much abdominal pressure that would bulge your pelvic floor downward. A bulging out belly means that your pelvic floor is also likely bulging outward. If this happens, try to scale the exercise back to a point where you can keep your abdomen more flat and EXHALE with the effort. And whatever you do, DO NOT worry about what your fitness instructor or trainer tells you to do if you CANNOT prevent the bulge!!! Communicate to them that you are protecting your body and that you need to scale back. Most personal trainers are NOT skilled in pelvic safe exercise. You HAVE to be your OWN ADVOCATE.
So if you think or know that you have POP, please do not despair. This issue is SO COMMON. You are NOT alone. Up to 50% of all women will have a POP to some extent in their lifetime.
The most important thing for you is to seek out a pelvic PT to help you work through your options. This may include a referral to a specialist surgeon for a consult as well. But there is SO MUCH you can do! Plus, the bonus of working on your POP is that you will likely see other benefits such as reduced back and hip pain, neck pain, and feel freer to do the activities you LOVE.