Gynecologic and abdominal surgeries are incredibly common. To give you an idea of HOW common, here are some numbers…
• Approximately 600,000 hysterectomies are performed annually in the United States.
• More than one million hernia repairs are performed each year in the U.S.
• Around 26% of first-time births are cesarean in the U.S.
• Approximately 280,000 appendectomies are performed each year in the U.S.
With these surgeries, there will be at least one incision ranging from a quarter of an inch to more than 4 inches in length into the abdomen for abdominal approach surgeries. Though constantly improving techniques are reducing the incision size, the reality is that the core muscles are disrupted. Unless an incision is only horizontal at the midline, then 4 layers of abdominal muscle will be cut.
Recovery instructions after these surgeries are usually to rest and minimize activity including heavy lifting for a few weeks ranging up to 12 weeks. But after that time, the patient is given the green light to return to normal activity. And it is not common or typical for these patients to be referred to a pelvic physical therapist (who specializes in core and pelvic floor muscles) or any therapy for that matter to help guide in optimal recovery and safe return to activity.
Questions that patients we see after abdominal surgery include:
-
How do I know if the scar is healing well?
-
How should I take care of the scar?
-
What if the scar hurts or feels like it is stuck and changing how I move?
-
How do I safely get back into my regular exercise routine?
-
What kind of abdominal exercises are safe for me to do?
-
How do I know if an exercise is too stressful on my body?
-
I feel disconnected from my core… how do I fix this?
-
I’m having new issues with (bladder leakage, low back pain, pelvic pain, constipation)… can this be helped?
Referring to the above common questions, physical therapists are well versed in monitoring wounds, scars, and guiding in the healing process. This can include helping with desensitizing sensitive scars as well as helping to improve the mobility of the scar tissue so that it does not create secondary issues related to fascial restrictions that can affect joints and soft tissue all the way into the shoulder, back, or even pelvic floor. Pelvic PTs will be more skilled in scars over the abdomen and pelvic floor.
Getting back to moving normally and returning to more vigorous activities and exercise after abdominal and gynecologic surgeries is also within the expertise of a pelvic PT.
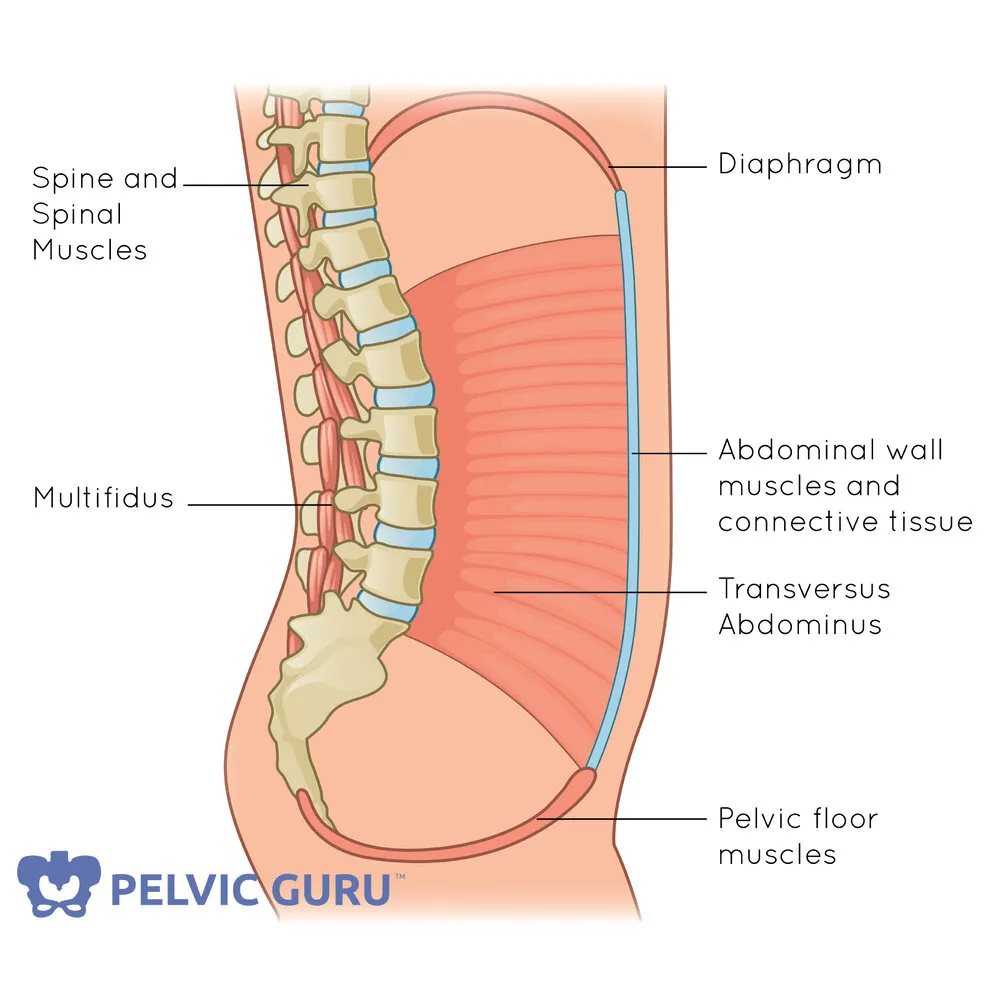
Regaining the connection and coordination between the deep core muscle system is crucial to returning to a full active life, free of low back pain, abdominal pain, and free of limitations. However, this does sometimes require guidance. Additionally, many patients may never have had good coordination within their deep core muscles, and only after a surgery, do they feel the effects of this. They may report feeling disconnected with their abdominals, or easily feel strained with simple activities. They may also experience an increase in pressure into the hernia repair or pelvic floor region with prolonged standing or lifting activities.
Pelvic PTs are experts at helping patients find their deep core and use these muscles effectively to lift without injuring their back, to sneeze without leaking urine, and to lift without straining the hernia repair or pelvic floor. And to manage emptying the bowels and bladder safely and effectively without needing to strain or have issues with not leaking.
Pelvic PTs often hear stories from our patients of prior surgical procedures where they had no postoperative guidance and feel the negative effects of this years later. Whether it is chronic pain or long-term body disconnect, these issues could have been avoided or greatly diminished if they had worked with a pelvic PT who specializes in core and pelvic floor health to help guide them on their healing journey.
Clearing someone to return to all “normal” activities should include more than screening for incision infections and significant pain. A pelvic physical therapist may only need to see the patient for 1-4 visits to ensure a full recovery, and the patient will be saved from sometimes years of frustration and even from a subsequent surgery.
Have questions? Contact us for a virtual consult with one of our pelvic PTs!